| Last updated on July 31, 2023
Medical adhesive related skin injuries (or MARSIs) are a dangerously common, but under recognized medical complication.
From premature infants to elderly patients with chronic-health conditions, MARSI occurs in all care settings and affects patients of all ages.
Yet, MARSIs are preventable – not inevitable.
In addition to dressing application and removal techniques, today there is new dressing technology that is gentle on the skin but tough when preventing infections.
Healing shouldn’t hurt – and it's time for hospitals to move beyond the traditional acrylic-based dressings that can create wounds, cause scarring and delay healing.
Keep reading to learn more about:
- What MARSI is
- Why MARSI happens
- How to prevent a MARSI
- The benefits of soft silicone dressings
Key takeaways:
- Skin is a natural barrier that protects us from infection, but many routine patient care interventions have a detrimental effect on the skin
- Threats to skin integrity are incredibly common, with 30% of cancer patients experiencing a MARSI
- Gentle adhesive dressings can help prevent pain and skin injuries, maintaining intact, healthy skin
What is MARSI?
A medical adhesive related skin injury occurs when medical adhesives – peeled away from raw, vulnerable skin – cause the surface layers of the skin to be torn.
Damage to the skin doesn’t just cause pain, trauma and ongoing discomfort, it can result in harmful bacteria finding their way into the skin tissues of surgical incisions, IV sites or the bloodstream.

Common symptoms of MARSI include:
- Dermatitis reactions where the skin appears red or develops a rash
- Allergic dermatitis where the skin becomes red with vesicles
- Maceration where the skin appears white or gray and becomes wrinkled
- Folliculitis where the hair follicles in the skin develop an inflammatory reaction
There are many types of skin infections like cellulitis that without further medical treatment will lead to serious health complications like bacteremia or endocarditis.
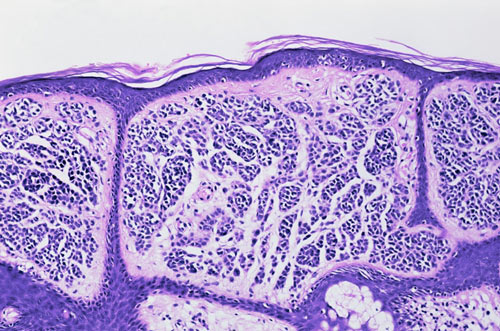
Skin’s protective barrier
Our skin is a barrier that protects us from infection, a natural bandage when we need to heal, and a receptor to feelings like pain or gentle touch. When our skin is wounded, that barrier is compromised, leaving us exposed and at risk of developing serious infections.
Sometimes, it’s medically necessary to break that barrier to perform life-saving surgeries, or to provide medical attention to vulnerable patients, such as oncology patients who require implanted vascular access ports to receive ongoing treatment.
When our skin needs assistance to heal, we use medical adhesives to help our skin mend – but many of the adhesives historically used in hospitals result in cringe-worthy dressing changes that can further damage skin that is already sore, thin and tender.
One of the most painful parts of a MARSI is when the skin torn or injured by medical adhesives still needs to be touched, poked or re-bandaged regularly.
Some vascular access sites can’t be moved to a different location depending on the form of treatment being administered, which means that these sites, no matter how painful they have become, must be covered with medical adhesives over and over again, leading to further pain and trauma to the skin.
If you’ve ever had to watch a child, loved one or patient receive treatment directly on top of a vulnerable skin wound, you know that this can be traumatizing for everyone involved.
In fact, studies show that nurses working with pediatric populations who experience chronic pain are at risk of developing:
- Moral distress
- Fear of losing compassion
- Negative views of the hospital environment
Why MARSI happens
Skin is the body’s largest organ and natural defense system. It contains a range of nerve endings which trigger responses to pain and trauma – or gentleness and affection.
MARSI can happen to anyone but certain populations who have or develop fragile skin during the course of their treatment are at increased risk.
Those who spend considerable time in a hospital environment know that it is not the most supportive environment for skin health due to dry air circulation and disinfectants used to prevent and control infections.

Causes of fragile skin may include, but aren’t limited to:
- Malnutrition
- Dehydration
- Mobility impairment
- Use of certain medications
- Treatments including chemotherapy, radiation therapy, immunotherapy and more
- Trauma such as a burn or injury
- Conditions like diabetes that can result in skin ulcers
- Pregnancy and menopause
- Prematurity
- Aging
When skin is already raw, damaged, and vulnerable, sticky medical adhesives being peeled away and replaced – often many times a day, every day – can lead to MARSIs, pain, trauma, anxiety, and chronic distress.
Frequent and painful dressing changes
Risk of MARSI increases with repeated removal and application of medical adhesives, leaving patients with long-term health complications more likely to develop MARSI.
Long-term use of medical adhesives in Pediatric ICUs result in a high risk of MARSI, most commonly skin stripping, due to frequent removal and application of medical adhesives.
Medical professionals who work in pediatric or neonatal Intensive Care Units (ICUs) know that something as simple as changing a dressing on a baby can be a challenging experience when the dressing causes pain and skin damage.
In some settings, multiple care providers are required to physically hold pediatric patients down upon dressing removals - yet, it doesn’t need to be this way.
Preventing skin injuries reduces medical complications, improves patient satisfaction, and improves clinical outcomes.
What ingredients are in medical adhesives?
The ingredients of medical adhesives have a part to play in the development of medical adhesive-related skin injuries.
Most medical adhesive base ingredients are:
- Acrylic or cyanoacrylates
- Polyisobutylene (or synthetic rubber)
- Silicone
Acrylic-based medical adhesives are most commonly used in hospital settings. These traditional adhesives, though effective in sealing wounds or holding vascular access ports in place, can cause varying degrees of skin injury.
Preventing MARSI
Fortunately for health care professionals, patients, and loved ones alike – MARSI is preventable, not inevitable.
According to a study conducted by the International Journal of Nursing Studies Advances, the prevention of MARSI depends on:
- Screening of patients who have a history of sensitive skin or skin infections
- Proper medical adhesive removal and application processes
- The type of adhesive used on sensitive skin (standard acrylic-based adhesives may not work for skin which is very old, very young, and very sensitive)
- Education of health care professionals and patients about MARSIs
“Skin damage from traditional acrylic dressings can create life-threatening complications for patients, and place an extra burden on health care providers. Care providers and patients deserve – and now have access to – better care than the basic dressings currently used in many hospitals.”
Gentle alternatives to medical adhesives
Today, new dressing technology is designed with patient skin safety, comfort and compassion in mind.
Atraumatic adhesive products can successfully protect against complications of skin injuries and prevent infections.
Covalon’s silicone based dressings are associated with significantly less damage to the outer skin layer and less pain on removal, preserving skin integrity to help prevent infections.
Characteristics of silicone dressings include:
- Fluid retention and absorbency
- Adherence to skin without sticking to wounds
- Vapor permeability
- Atrumatic upon removal
Unlike acrylic dressings, soft silicone will not cause epidermal stripping or pain upon removal.
At a major Children’s Hospital in southern California which recently started using Covalon’s silicone based dressing IV Clear, a vascular access professional commented that the dressing was so gentle they were able to change a central line dressing without waking their pediatric patient, an incredible improvement to what can commonly be a very stressful experience to all involved.
Compassionate care technology like IV Clear reduces unwanted complications, improves patient outcomes, and supports stronger patient-clinician relationships.
If you’re interested in experiencing the difference of soft silicone yourself, request a free sample today, and experience how gentle and effective Covalon’s products are for yourself.
References
Journal of Pediatric Psychology: Burnout in Nurses Working with Youth With Chronic Pain
National Library of Medicine: Medical adhesive-related skin injuries
National Library of Medicine: MARSI in Pediatric Intensive Care Unit
National Library of Medicine: MARSI Prevalence in Adult Acute Care Settings
National Library of Medicine: Contact Dermatitis and Medical Adhesives
International Journal of Nursing Studies Advances: Prevention of MARSI during patient care

Katherine is Senior Director of the Clinical Affairs Department at Covalon Technologies which works directly with clinician, patient, and caregiver stakeholders to offer innovative compassion-driven solutions.
















