| Last updated on January 24, 2024
Vascular access nurses play a critical role in ensuring the safe and effective delivery of medical treatments through vascular access devices – the most common of these being peripheral intravenous lines.

These specialized healthcare professionals play a vital part in modern medicine, enabling their fellow clinicians to have reliable access to patients' bloodstreams for various procedures and therapies.
However, vascular access nurses can face numerous patient care challenges, including the risk of infections, coordination complexities, and the need to keep up with evolving technologies. Fortunately, advanced vascular access technology is now available, not only providing protection against infections and offering compassionate solutions for skin sensitivities and issues, but also making the job of vascular access nurses easier and improving overall patient care
In this article, we will dive into the world of vascular access nurses and vascular access specialists, exploring their vital roles, the obstacles they encounter, and how compassionate medical technology can revolutionize patient care in this critical specialization.
Keep reading to find out:
- What is a vascular access nurse?
- What do vascular access nurses do?
- Challenges that vascular access teams face
- Special technology for vascular access teams
What is a vascular access nurse?
A vascular access nurse is a highly specialized healthcare professional with specialized training and expertise in managing vascular access.
Vascular access is the insertion and maintenance of vascular access devices that are used to access the bloodstream, such as intravenous (IV) catheters, and other devices used to deliver medications, fluids, and perform various medical procedures.
Vascular access nurses play a crucial role in ensuring that doctors and nurses have safe and effective access to their patients’ bloodstreams – a vital aspect of modern healthcare.
The primary focus of a vascular access nurse is to prevent complications, such as infections or clotting, while maintaining safe and stable access to a patient’s bloodstream.
Vascular access nurses are vital in a range of clinical scenarios, providing expert care in situations including, but not limited to:
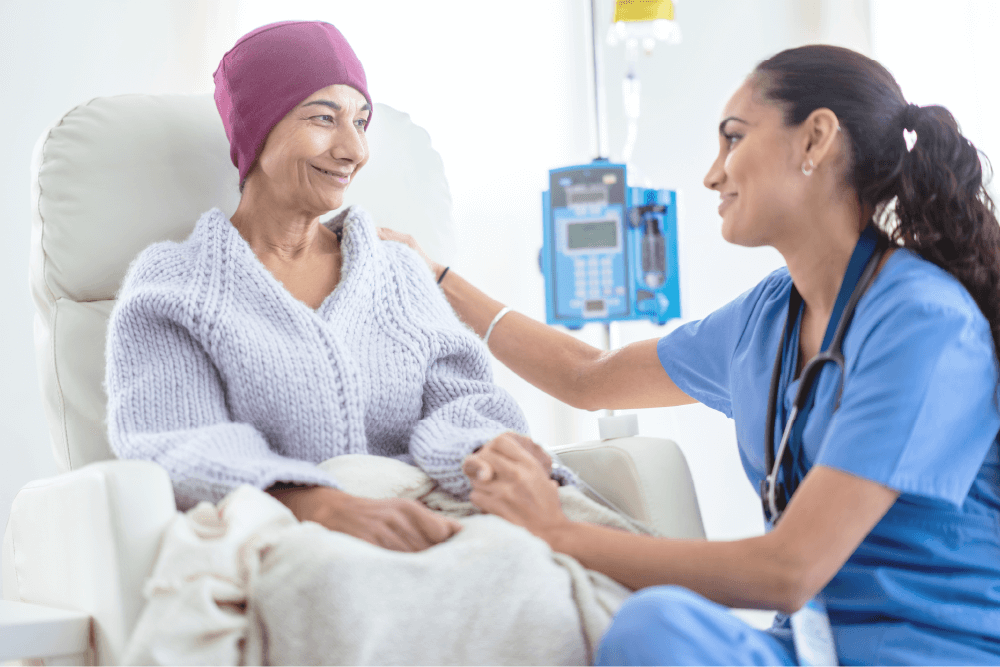
- Patients Requiring Long-term IV Therapy: Such as those with chronic diseases requiring regular medication infusion, including chemotherapy for cancer patients.
- Individuals with Difficult Vein Access: Patients who have challenging vein access due to various conditions like obesity, dehydration, or a history of intravenous drug use.
- Patients Needing Frequent Blood Draws: Those who require regular blood tests, like individuals with chronic kidney disease undergoing dialysis.
- Neonatal and Pediatric Patients: Infants and children who need extra specialized care for IV line placements due to their small and delicate veins.
- Elderly Patients: Older adults with fragile veins and skin who require gentle and expert handling for IV insertions and maintenance.
- Patients Undergoing Major Surgeries: Individuals who need central lines or other complex vascular access devices for perioperative fluid and medication management.
- Critically Ill Patients in Intensive Care Units (ICU): Those in critical condition who may require multiple lines for medication, nutrition, and monitoring.
- Patients with Infections Requiring Intravenous Antibiotics: Such as those with severe infections where oral medications are not effective.
- Individuals with Limited Mobility: Patients who might have complications in maintaining peripheral IV lines due to mobility issues.
Vascular access nurses work on vascular access teams with other vascular access specialists.
What is a vascular access specialist?
A vascular access specialist team consists of medical professionals who receive advanced knowledge and training regarding insertion techniques, clinical care, and management of peripheral vascular access devices.
General medical teams that include nurses and doctors of other specialities may also have knowledge about insertion techniques, however vascular access specialists are specifically trained on advanced insertion techniques, and are particularly qualified to care for vascular access devices.
What is a vascular access specialist team?
Members of a vascular access team are typically responsible for the assessment, insertion, and management of vascular access devices for patients who require medical treatment through vascular access, especially central venous catheters.
These specialists typically have extensive training in techniques and technologies related to vascular access devices, such as:
- Central venous access devices
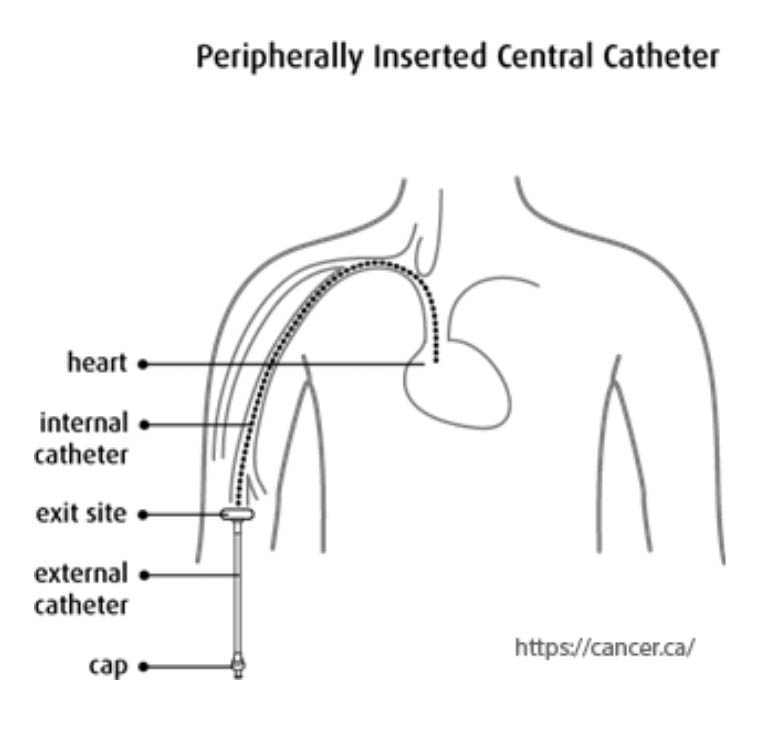
- Peripherally inserted central catheters (PICC lines)
- Arteriovenous (AV) fistulas and other vascular access methods
- Care & Maintenance of venous access devices
- Infection prevention
The expertise of a vascular access team helps to improve patient outcomes by minimizing the risks associated with vascular access procedures, such as failed catheter insertions or complications - like catheter-related bloodstream infections (CRBSIs) - which can be caused by improper insertion or maintenance of catheters.
Also read: Central line care: Protection against Healthcare Associated Infections (HAIs)
What do vascular access nurses do?
Vascular access nurses and specialists are responsible for various critical tasks related to vascular access.
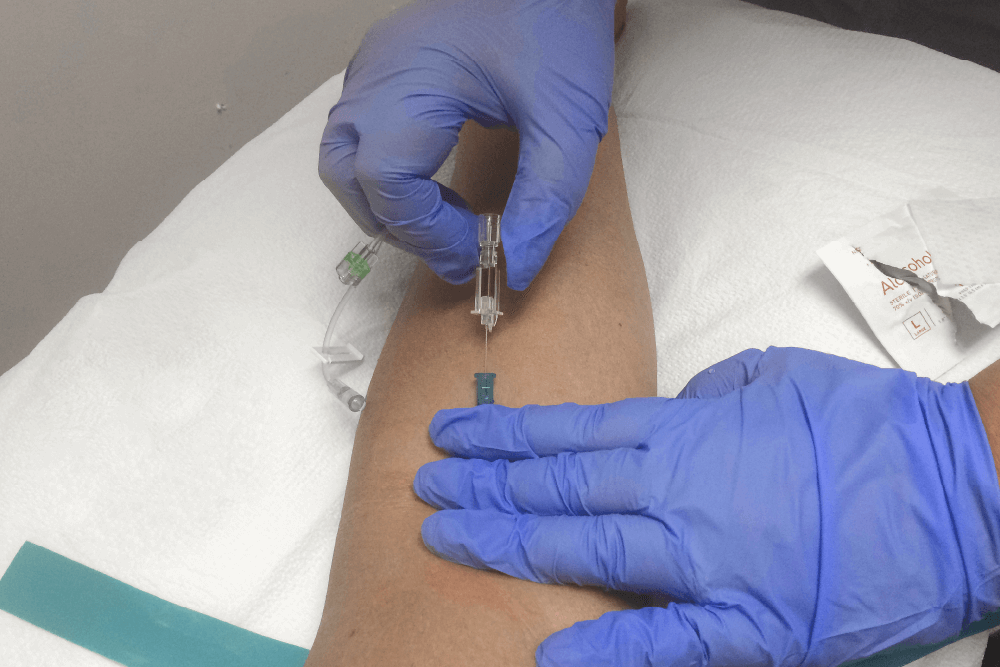
They assess patients' vascular access needs, select appropriate devices based on individual requirements, and skillfully insert these devices while ensuring patient comfort and safety.
These professionals also monitor and maintain vascular access sites, preventing complications like infections and thrombosis (the clotting of blood vessels).
Additionally, they educate patients and healthcare teams on best practices for vascular access care, promoting patient awareness and participation in their own treatment.
Bedside nursing and vascular access care
Exceptional nurses of every medical department practice bedside nursing - the compassionate, holistic care of patients in which they provide physical, emotional, and psychological support.
Vascular access nurses are involved in the daily care of patients who are in need of or connected to an IV line. As such, their care of patients has a large and direct effect on the patient experience while hospitalized.
Compassionate nursing is made easier when hospitals and healthcare units are equipped with medical devices that make compassionate care a priority.
Challenges that vascular access teams face
There are many challenges that a vascular access nurse may face during the course of any given day.
One common issue is the risk of infection associated with vascular access devices, which requires vigilant infection control measures.
Vascular access specialists also need to navigate the complexities of coordinating care among various healthcare providers and ensuring the timely removal of unnecessary devices to minimize complications.
They must also stay up to date with evolving technologies and best practices in vascular access, which can be demanding in an ever-changing healthcare environment.
Challenges for vascular access nurses in providing patient care
Depending on the geographic location of the vascular access specialist team, the hospital they work in, and typical demographics of patients they typically work with, a vascular access nurse may face a variety of challenges in providing medical care on a daily basis.
- Vascular access teams may encounter challenges related to healthcare disparities, where certain patient populations, especially those from underserved communities or with limited access to healthcare, may have higher rates of complications related to vascular access. Addressing these disparities and ensuring equitable access to specialized care can be a unique challenge.
- Providing vascular access in pediatric patients presents distinct challenges due to their smaller veins, limited tolerance for discomfort, and the need for specialized equipment and techniques. Vascular access teams that work with children must be well-trained in pediatric-specific procedures and be adept at addressing the unique emotional and psychological needs of pediatric patients and their families.
- Some patients may have complex medical conditions or comorbidities that make vascular access particularly challenging. This can include patients with obesity, severe edema, or vascular diseases that affect their vasculature. Vascular access teams need to develop specialized strategies and adapt their approaches to ensure safe and effective access in these cases.
In emergency or trauma settings, rapid and reliable vascular access is critical for life-saving interventions. Vascular access teams working in trauma centers may face challenges related to extreme time pressures, difficult vascular access due to injuries, and the need to coordinate with multiple healthcare providers simultaneously. The ability to efficiently navigate these high-stress situations is a niche challenge for such teams.
Organizational level challenges faced by vascular access nurses
Regardless of which medical unit vascular access nurses are working in, there are corporate challenges that many vascular access teams may face.
- Lack of funding for best-in-class, compassionate medical devices. In some hospitals, the funding may not be available to invest in compassionate medical devices, such as gentle adhesives that don’t tear skin, or clear IV dressings that make IV line monitoring easier for vascular access nurses. This leaves vascular access nurses with fewer options for patients requiring specialized care, forcing them to rely on traditional devices and medical dressings which may increase the risk of complications such as skin damage.
- Lack of support from acquisitions managers to invest in compassionate technology. In some cases, even if the funding exists, those responsible for product selection and procurement may not see the need to invest in certain medical devices that can help vascular access nurses to provide top-notch care to their patients.
- Lack of internal support for nursing staff. A lack of managerial support may lead to healthcare worker burnout. Nurses who are experiencing burnout are less likely to be able to show compassion in their work with patients, and are less likely to have the energy to advocate for compassionate technology on patients’ behalf.
Up next: Watch this Webinar on why protecting skin integrity is key to infection prevention.
Special technology for vascular access teams
Investing in world-class compassionate medical devices should be the standard of care for all medical facilities – especially in vascular access settings.
Vascular access nurses are responsible for managing the direct line that connects a patients’ bloodstream to their access to life-saving medical treatment.
Patients should be able to trust that they’re getting the best care possible to help protect against infections and complications while receiving care – and vascular access specialist teams should be able to trust the vascular access medical devices they are using.
How to choose compassionate medical devices
When medical staff can’t find a dressing that works – they typically come to Covalon.
As a leading innovator in the field of advanced wound care and infection prevention technologies, our medical devices, including antimicrobial dressings and securement devices, are designed to address the unique challenges faced by vascular access teams.
Explore our industry-first Vascular Access Technologies for secure, protective and patient-friendly solutions in IV care and management.
| IV Clear | CovaClear | VALGuard |
|

|

|
These technological advancements play a pivotal role in enhancing the efficiency and safety of vascular access procedures, ultimately benefiting both patients and healthcare providers.
Healing shouldn’t hurt – and Covalon’s gentle vascular access dressings can help to reduce pain and worry during dressing changes - providing some relief.
Try the Covalon challenge – request free samples and experience our gentle vascular access dressings compared to traditional adhesive medical dressings for yourself.
Resources:
National Library of Medicine: Vascular access specialists
National Kidney Foundation: Hemodialysis access
Canadian Cancer Society: Central venous catheters
KidsHealth: Peripherally inserted central catheter (PICC line)





















